Title: Corruption in Healthcare: An In-depth Analysis of Challenges and Solutions in the United States
Abstract:
Corruption in healthcare is a multifaceted issue that undermines the integrity of healthcare systems, erodes public trust, and compromises patient outcomes. In the United States, despite stringent regulations and oversight mechanisms, instances of corruption persist, ranging from fraudulent billing practices to conflicts of interest among healthcare professionals and industry stakeholders. This essay provides a comprehensive examination of corruption in healthcare within the context of the United States, exploring its root causes, manifestations, and consequences. Drawing on empirical research, case studies, and expert insights, it identifies systemic vulnerabilities and institutional failures that contribute to corruption, while also highlighting promising strategies and reforms aimed at combating unethical behavior and promoting transparency, accountability, and ethical integrity in the healthcare sector.
Introduction:
The integrity of healthcare systems is fundamental to ensuring equitable access to quality care, safeguarding patient safety, and upholding public trust. Corruption in healthcare poses a significant threat to these principles, compromising the delivery of services, distorting resource allocation, and impeding efforts to improve health outcomes.

In the United States, corruption in healthcare manifests in various forms, including kickbacks, bribery, embezzlement, and conflicts of interest, among others. Despite regulatory frameworks and enforcement mechanisms aimed at preventing and addressing corruption, challenges persist, underscoring the need for sustained vigilance and reform efforts.
Root Causes of Corruption in Healthcare:
Understanding the root causes of corruption in healthcare is essential for devising effective strategies to combat unethical behavior and promote integrity within the system. Several factors contribute to the prevalence of corruption, including:
- Financial Incentives: The fee-for-service reimbursement model incentivizes healthcare providers to maximize billable services, potentially leading to overutilization, unnecessary procedures, and fraudulent billing practices.
- Complex Regulatory Environment: The complexity of healthcare regulations creates loopholes and ambiguities that can be exploited by unscrupulous individuals and organizations for personal gain.
- Lack of Transparency and Accountability: Insufficient transparency and oversight mechanisms enable corruption to flourish by shielding illicit activities from scrutiny and accountability.
- Conflicts of Interest: Relationships between healthcare providers, pharmaceutical companies, medical device manufacturers, and other industry stakeholders can create conflicts of interest that compromise clinical decision-making and patient care.
- Cultural Norms and Perceptions: Societal attitudes toward corruption, tolerance of unethical behavior, and perceptions of impunity can influence the prevalence of corrupt practices within the healthcare sector.

Manifestations of Corruption in Healthcare:
Corruption in healthcare can take various forms, each with its own implications for patient care, resource allocation, and public trust. Common manifestations of corruption include:
- Billing Fraud and Abuse: Healthcare providers may engage in fraudulent billing practices, such as upcoding, unbundling, and billing for services not rendered, to inflate revenues and maximize reimbursement.
- Kickbacks and Bribery: Pharmaceutical companies, medical device manufacturers, and other industry stakeholders may offer kickbacks or bribes to healthcare providers in exchange for preferential treatment, prescribing their products, or influencing purchasing decisions.
- Embezzlement and Financial Mismanagement: Administrators, executives, and employees within healthcare organizations may embezzle funds, misappropriate resources, or engage in financial misconduct for personal enrichment.
- Conflict of Interest: Conflicts of interest can arise when healthcare providers have financial or non-financial relationships with industry stakeholders that may influence their clinical judgment, research findings, or professional conduct.
- Regulatory Capture: Regulatory agencies tasked with overseeing the healthcare industry may be susceptible to regulatory capture, where industry interests outweigh public health and safety considerations, leading to lax enforcement and inadequate oversight.
Consequences of Corruption in Healthcare:
The consequences of corruption in healthcare are far-reaching and profound, affecting patients, providers, and society at large. Some of the key consequences include:
- Compromised Patient Care: Corruption can undermine the quality and safety of patient care by incentivizing unnecessary procedures, substandard treatment, and biased decision-making driven by financial interests rather than clinical need.

- Erosion of Public Trust: Instances of corruption erode public trust in the healthcare system, leading to skepticism, disillusionment, and decreased confidence in the integrity and reliability of healthcare services.
- Waste of Resources: Fraud, waste, and abuse divert scarce resources away from patient care, research, and public health initiatives, impeding efforts to address pressing health challenges and improve health outcomes.
- Inequitable Access to Care: Corruption can exacerbate disparities in access to healthcare by diverting resources away from underserved communities, perpetuating inequalities, and exacerbating health inequities.
- Undermining Professional Ethics: Corruption undermines the ethical principles and professional standards that govern the practice of medicine, eroding the integrity of healthcare professions and diminishing public trust in healthcare providers.
Strategies to Combat Corruption in Healthcare:
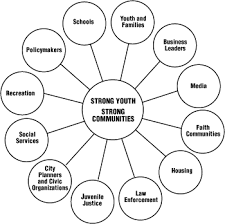
Addressing corruption in healthcare requires a multifaceted approach that addresses root causes, strengthens regulatory frameworks, promotes transparency, and fosters a culture of ethical integrity. Some key strategies include:
- Enhanced Oversight and Enforcement: Strengthening regulatory oversight and enforcement mechanisms to detect and deter corrupt practices, including increased scrutiny of billing practices, whistleblower protections, and sanctions for misconduct.
- Transparency and Accountability: Promoting transparency in healthcare transactions, financial disclosures, and industry relationships to mitigate conflicts of interest, enhance public trust, and hold stakeholders accountable for their actions.
- Ethics Training and Professional Development: Providing healthcare professionals with education and training in medical ethics, professionalism, and conflict-of-interest management to uphold ethical standards and navigate ethical dilemmas effectively.
- Whistleblower Protections: Establishing robust whistleblower protection mechanisms to encourage individuals to report instances of corruption, fraud, and misconduct without fear of retaliation and ensuring thorough investigation and follow-up.
- Promotion of Value-Based Care: Shifting toward value-based care models that prioritize quality, outcomes, and cost-effectiveness over volume-driven reimbursement incentives to align financial incentives with patient-centered care and promote efficiency and accountability.

Influences:
- Pharmaceutical Industry Influence: The pharmaceutical industry’s influence on healthcare policy, research, and clinical practice has been a subject of scrutiny regarding potential conflicts of interest and undue influence. Pharmaceutical companies often engage in aggressive marketing tactics, including direct-to-consumer advertising and financial incentives for healthcare providers, which can impact prescribing patterns and contribute to overutilization of medications.
- Medical Device Industry Practices: Similar to the pharmaceutical industry, the medical device industry faces concerns about transparency, conflicts of interest, and regulatory capture. Device manufacturers may influence clinical decision-making through financial relationships with healthcare providers, sponsorship of research studies, and lobbying efforts aimed at shaping regulatory policies.
- Healthcare Fraud Enforcement: While the U.S. has robust enforcement mechanisms to combat healthcare fraud, including the False Claims Act and the Anti-Kickback Statute, challenges remain in detecting and prosecuting fraudulent activities effectively. Coordination among federal agencies, such as the Department of Justice and the Office of Inspector General, is crucial for investigating complex cases of healthcare fraud and holding perpetrators accountable.
- Data Privacy and Security Concerns: The increasing digitization of healthcare data introduces new risks related to data privacy and security, including the potential for corruption through unauthorized access, data breaches, and misuse of patient information. Strengthening cybersecurity measures and regulatory safeguards is essential for protecting patient privacy and preventing corruption-related breaches.
- Political Influence on Healthcare Policy: Political contributions, lobbying efforts, and industry-funded research can influence healthcare policy decisions, shaping regulatory frameworks, reimbursement policies, and public health initiatives. Addressing the influence of money in politics and promoting transparency in campaign finance can help mitigate the risk of corruption in healthcare policymaking.
- Global Perspectives on Corruption in Healthcare: Comparing corruption in the U.S. healthcare system with practices in other countries provides valuable insights into common challenges, best practices, and lessons learned. Cross-national studies and collaborations can inform strategies for addressing corruption globally and promoting international cooperation in combating unethical practices in healthcare.
- Patient Advocacy and Consumer Empowerment: Empowering patients and consumer advocacy organizations to demand transparency, accountability, and ethical conduct in healthcare can serve as a powerful deterrent against corruption. Educating patients about their rights, promoting shared decision-making, and facilitating access to information can help counteract asymmetric power dynamics and promote patient-centered care.

- Healthcare Workforce Integrity: Ensuring the integrity of the healthcare workforce requires robust recruitment, training, and oversight mechanisms to prevent corruption, fraud, and abuse among healthcare professionals. Implementing rigorous background checks, ethical standards, and professional codes of conduct can help maintain high ethical standards and promote trust in healthcare providers.
Conclusion:
Corruption in healthcare poses significant challenges to the integrity, efficiency, and equity of healthcare systems, undermining patient care, eroding public trust, and impeding efforts to improve health outcomes. Addressing corruption requires a concerted effort to address root causes, strengthen regulatory oversight, promote transparency, and foster a culture of ethical integrity within the healthcare sector. By implementing comprehensive reforms and adopting evidence-based strategies, stakeholders can combat corruption, uphold ethical standards, and safeguard the integrity of healthcare systems in the United States and beyond.